PROJECT FOCUS: Using Personal Health Budgets to address inequalities and support people severely affected by mental illness achieve their recovery goals
LEAD PARTNERS: City & Hackney Psychological Therapies & Wellbeing Alliance members, including Core Arts & Sports, The Advocacy Project and East London Foundation Trust, with support and guidance from NHS England Personalised Care leads
What can help me get well and stay well?
What Matters To Me: Using Personal Health Budgets for Mental Health Recovery
City & Hackney has one of the UK’s highest prevalence of Severe Mental Illness (SMI), compounded by high deprivation, digital exclusion, and fragmented mental and physical health support.
Feedback from dedicated service user groups flagged that many people severely affected by mental illness were unable to achieve their recovery goals and be discharged from secondary services to primary care. Meanwhile, national policy around personalisation and digital transformation in mental health was advancing, creating an opportunity to redesign care around the individual.
We worked with our service users to redesign the recovery planning process along the whole recovery pathway. As programme lead, I was tasked with designing and delivering a cross-sector pilot that would embed low cost, direct payment Personal Health Budgets (PHBs) in the recovery pathway as a means of achieving individual goals, and also bridging income inequalities.
I led co-production workshops with service users, clinicians and commissioners, applying a strengths based model to recovery goal setting. I developed the strategy to scale PHBs beyond s117 across the whole pathway, embedding them in digital care plans and designed a tiered authorisation system to ensure equity, governance and support and training materials for staff. I also designed and launched the “Stay Connected” PHB to provide devices and connectivity to those at risk of exclusion.
As a result, we became the first site in England to offer PHBs across the whole SMI recovery pathway, not just 117 aftercare, and where PHBs are integrated into digital personalised care planning, supporting people to self-manage their mental wellbeing and step-down to primary care.
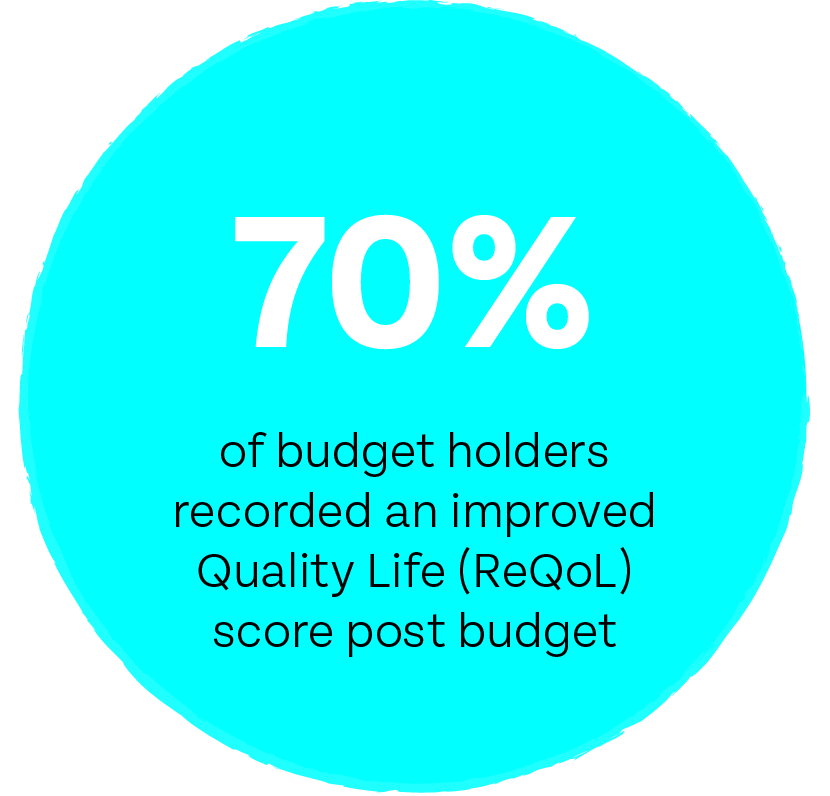
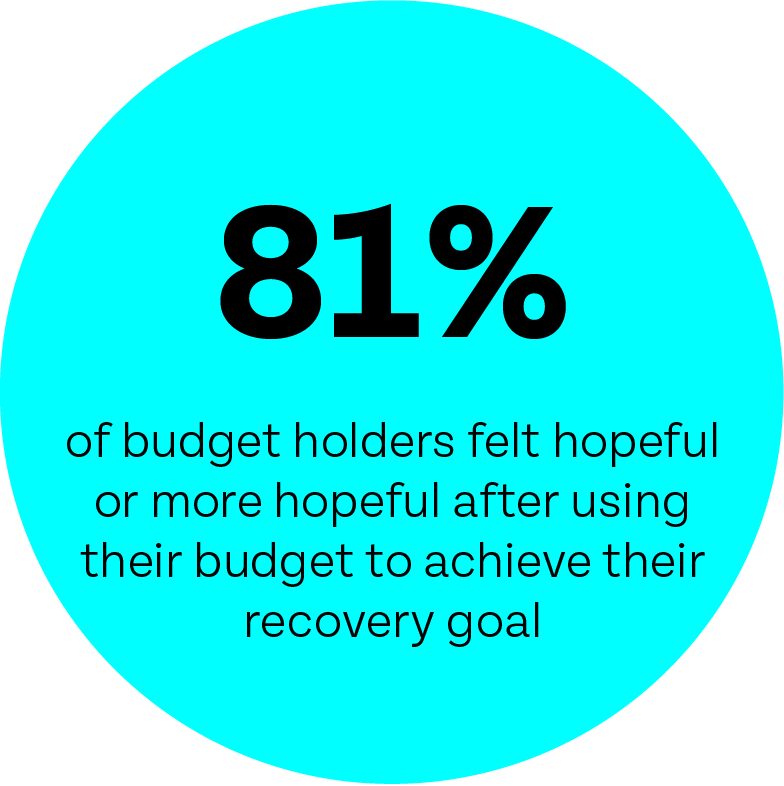
To date, almost 3,000 one-off budgets have been accessed across 40 mental health teams in City & Hackney, Tower Hamlets & Newham to date with the following outcomes achieved:



Case study: The kite flyer
Abdul was in recovery for PTSD and dissociative disorders. After he was discharged from hospital he was living in the community, having regular psychotherapy and was an active member of a support group. Although he felt emotionally stable he expressed to his care co-ordinator that he experienced a sense of disconnect to himself and his life.
He was particularly worried about forgetting his memories of his home country, his childhood and family back home. His post-traumatic stress was connected to what he’d experienced in Afghanistan and it was difficult for him to think about his family or home country without stressful memories bubbling up or worse drawing a blank. His care co-ordinator wondered if he could recall any times he’d felt good in Afghanistan, perhaps when he was a child? Abdul remembered being an avid kite flyer as a child. He loved the way it made him feel. He’d been good at it and even had the skills to steer his kite in competition.
A small PHB was used to enable the purchase of a kite. Abdul said he loved flying the kite and it had given him a positive way to connect with his past, his sense of identity and home country. He was also going to the park more and had met another kite flyer.
He said he felt happier after receiving the PHB than he was before.
“My identity used to be very connected to my mental health, but since having a PHB my identity is now primarily as an artist. I’ve had private views and my work’s been shown at festivals and in the media.”
PHB recipient Hackney
I have a project that I want to do for my dog Ruby, who passed away this year. This project will be a memorial for her and will help me in the healing process.
I am making red ceramic hearts to leave in different places and parks that hold memories of her for me. I was homeless with her for eight years and we walked all over London together. Revisiting the places we went together and leaving ceramic hearts is the best way for me to honour those memories.”
Christian, Recovery Goal: To manage bereavement
Chris’s PHB Journey
Chris has schizoid affective disorder and whilst he has things in place that support his recovery, including regularly attending music classes at Core Arts, commissioned to provide recovery services in the community. He found that when he was at home on his own he was most vulnerable to hearing voices.
When he spoke with his care co-ordinator about what was working and what wasn’t working at the moment they figured out that perhaps he needed a bit more support in this area. This helped him identify a more specific outcome.
Instead of his goal being to ‘stay out of hospital’ he wanted to ‘stop the voices when I’m at home. The PHB supported purchase of an electric guitar to use at home.
Chris: “having the electric guitar has changed my life, I am not scared of the voices anymore as I know what to do when they start up.”
Chris’s Care Co-ordinator: “Chris’s PHB has been really successful – not only can he now manage his symptoms himself, but is amazing at the electric guitar!”

PUBLICATIONS, CITATIONS & AWARDS
PUBLICATION
Evaluation of Mental Health Personal Health Budgets
National Development Team for Inclusion (NDTi)
PUBLICATION
A review of Personal Health Budgets for people from Black and minority ethnic communities
Race Equality Foundation
Finalist:
Innovation & Improvement in Reducing Healthcare Inequalities
HSJ Awards 2022